When we use the word ‘asynchronous’ in terms of healthcare, we mean communication or care delivery that does not happen simultaneously.
For patients, this can mean submitting a query or care request through an online portal or app at any time that can then be reviewed by the GP or hospital and responded to at a later time.
This has become increasingly prevalent in order to triage general healthcare inquiries and manage initial appointments, and the use of the NHS app to provide a ‘digital front door’ for patients is a core part of the UK Government’s plan to reform elective care as published earlier this year.
The use of asynchronous communication in healthcare is not limited to interactions between health providers and patients, it is also used between clinicians to discuss patient cases, manage referrals, review information, and collaborate on patient care.
This is particularly important to help address some of the inbuilt delays to the patient journey in existing analogue models, such as test results and scans needing to wait until the next available multi-disciplinary team meeting to be discussed.
As part of the government’s targets for the NHS, all integrated care boards (ICBs) are being asked to improve referral to treatment times by at least 5% by March 2026, and reduce the number of patients waiting no longer than 18 weeks for elective treatment to 65% nationally.
However, these efficiency targets come alongside guidance to “live within their budgets” – which means delivering more productivity with existing staff and facilities. Efficiencies will need to be found in ways of every day working.
Asynchronous healthcare can help to drive these efficiencies in a number of ways.
How is asynchronous healthcare used in practice?
- Messaging: Utilising clinical communication platforms like Bleepa®, clinicians can discuss patient cases and request advice and guidance from colleagues. These can then be reviewed and responded to without disrupting existing work at a time that is convenient. This can be particularly beneficial for multi-disciplinary team (MDT) working where face-to-face meetings can mean delays in diagnosis and treatment.
- Adding data to patient records: Clinicians can upload reports, diagnostic results or other key clinical data to a digital patient record, meaning that all the relevant information about a patient is in one secure place and can be reviewed together with any communication.
- Image sharing: Clinicians can capture and send images, such as medical photography or other medical imaging, enabling colleagues to review, monitor and determine the best course of action.
- Pathway management: By being able to see all patient data in one place and review any communication around care, clinicians can also take an overview of a patient’s care and where they are on a patient pathway, manage referrals and update colleagues to keep everyone involved up to date.
Benefits of asynchronous healthcare:
- Flexibility: Instead of being restricted to discussing patient care when colleagues are available clinicians can communicate around their existing worklists, and where possible, also continue to work remotely and across sites using devices like tablets or mobile phones. Additionally, communication can happen the moment test results are available rather than having to wait for scheduled meetings. This also opens up the ability for clinicians to work across geographical regions.
- Accessibility: Clinicians can collaborate on patient care remotely and in underserved areas where real-time collaboration may be more challenging due to limited internet connectivity, travel or other logistical barriers.
- An auditable record: Asynchronous working can provide a digital record of the discussion around a of the patient’s status and the clinicians’ recommendations. Some tools allow for messages, images, and updates to be documented in real time, which can ensure an auditable record of care is maintained, reducing the risk of miscommunication or missed details.
- Improved staff experience: Clinicians are used to using asynchronous platforms to communicate in their day-to-day lives and can benefit from being able to communicate with colleagues conveniently and remotely, even when working in the same care setting.
Evidence of benefits – can asynchronous working save time?
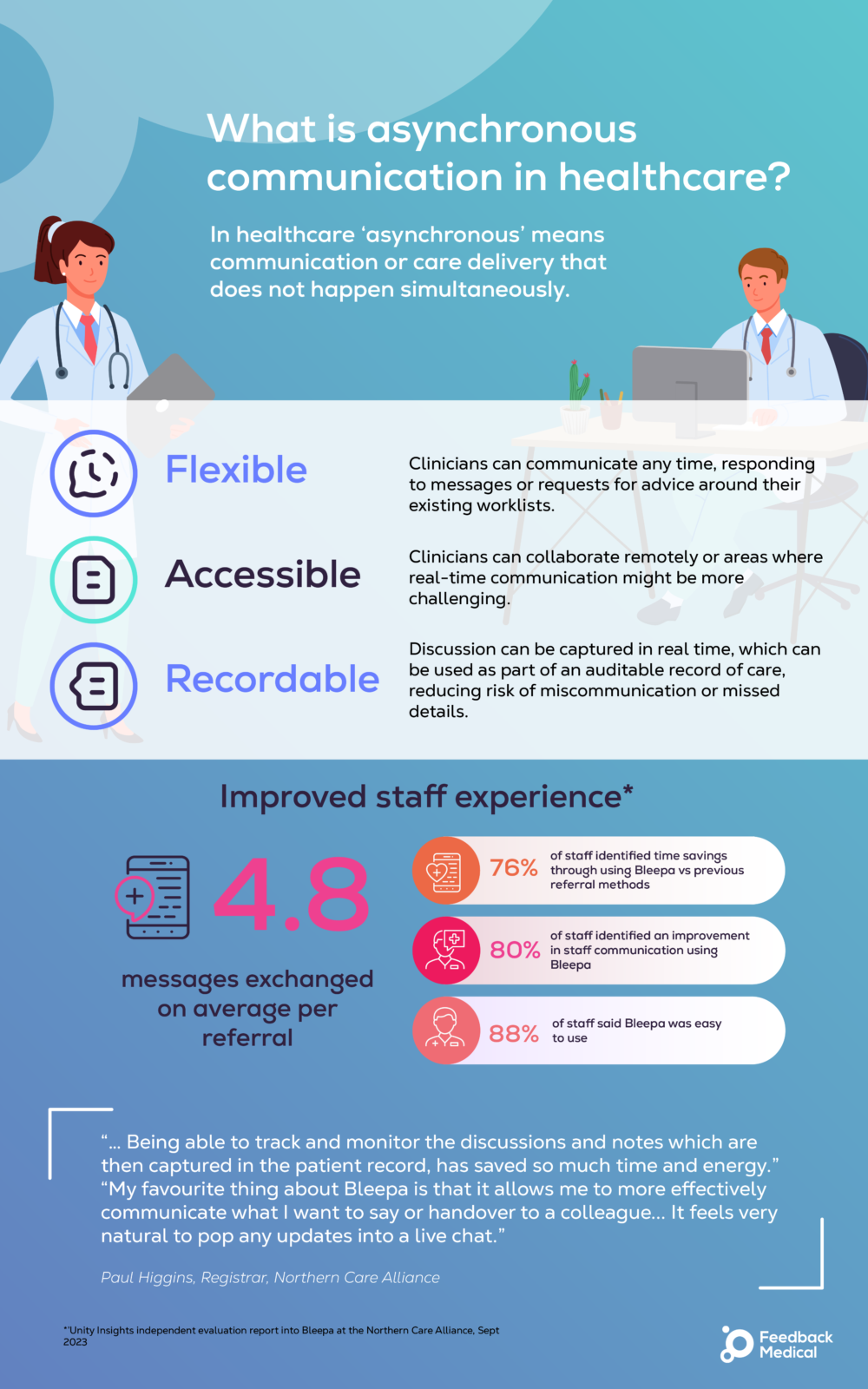
An independent evaluation of Bleepa® at the Northern Care Alliance supported the benefits of asynchronous care in speeding up patient referrals and handling communication between clinicians.
Referral response times in the respiratory specialty were reduced by 87% to 0.28 days on average compared to the average identified in a previous study.
Additionally, 80% of surveyed staff identified an improvement in communication when using Bleepa compared to previous referral methods, and 76% of staff identified time savings from using the platform.
“My favourite thing about Bleepa is that it allows me to more effectively communicate what I want to say or handover to a colleague… It feels very natural to pop any updates into a live chat.”
Registrar, Northern Care Alliance
For our digital breathlessness pathway with Queen Victoria Hospital NHS Foundation Trust, the use of Bleepa®’s asynchronous functions for multi-disciplinary discussion, combined with the connection of care settings across primary, secondary and community diagnostic centres, helped streamline the sharing of patient information and allowed for faster decision-making.
These efficiency benefits were fed through to patients, realising a 63% reduction in patient wait times compared to the 18-week national target, cutting the average time to 46 days from 126 days.
It is easy to refer patients onto the pathway and to discuss and respond to the GPs with our recommendations.”
Consultant in Sleep and Respiratory Medicine, Queen Victoria Hospital
Outside of our own findings, studies more broadly of asynchronous communication tools have supported the potential for time saving benefits for clinicians.
A study conducted in 2020 into the use of asynchronous communication at West Suffolk NHS Foundation Trust compared to previous methods showed a 59% time saving in average task completion for clinicians.
In that study, 70% of clinicians surveyed said the use of an asynchronous platform had improved interprofessional communication.
For time stretched clinicians, ways to communicate with colleagues quickly, remotely, and flexibly can support their workload, however, such tools face challenges in terms of their wider adoption and use by our healthcare system.
The challenges of asynchronous healthcare
- Clinical limitations: Some medical conditions may still require in-person assessment or real-time evaluation to provide accurate diagnoses or treatment plans.
- Complex cases: Whilst asynchronous communication can allow for multi-disciplinary discussions to happen outside of traditional MDT meetings, .
- Integration with existing systems: Clinicians use a number of different systems for clinical data, often with different systems used for medical imaging, diagnostic results and more; these are often not uniform across hospitals and might not integrate with one another or with electronic patient records, creating an incomplete picture of a patient.
- Privacy and security: Sharing sensitive health data through digital platforms raises concerns around patient privacy and data security. To comply with regulations, asynchronous communication platforms must meet stringent security standards to protect patient data from unauthorized access or breaches. Platforms that clinicians might use for asynchronous communication in their daily lives such as WhatsApp are not suitable for clinical discussions.
- Technological limitations: Not all clinicians have the same access to devices to use asynchronous tools remotely and flexibly; the application of bring-your-own device policies vary from hospital to hospital, and in some cases basic infrastructure such as access to wi-fi may be limited.
The good news is that some of these challenges can already be addressed by tools like Bleepa®.
Whilst messaging tools can allow for quick and flexible clinical discussions, these can only facilitate faster decisions if they can happen alongside the right patient data. By integrating with a number of clinical systems that pull together reports, diagnostics and medical imaging into a single digital health and diagnostics record, Bleepa® ensures that clinicians can collaborate with all the data they need to discuss a patient’s case.
Bleepa® is also certified for DICOM image viewing, meaning that images can be displayed at a suitable quality for clinical review, ensuring patient safety and reducing inadvertent risk for clinicians. Furthermore, no data is held on any device, but secured in a patient-centric cloud architecture to ensure data is protected.
While tools like Bleepa® can address many of the challenges from a technological and operational perspective, broader system-wide action is needed to realise the potential gains from asynchronous healthcare to support government productivity goals.
This includes bolstering digital infrastructure as a foundation for new technologies, clear approaches for the funding, procurement and deployment of digital collaboration tools, and support for clinicians to adopt new ways of working that make the most of them.
A focus on better use of technology is a major priority outlined by the government and is expected to be a key theme of the upcoming NHS 10-year-plan as part of broader aims to shift from analogue processes to digital.
Conclusion:
Asynchronous communication is being embraced to improve the ways in which patients and healthcare providers interact and provide better access and quality of healthcare delivery. To deliver the best impact, however, this also needs to be adopted between clinicians throughout all parts of the patient pathway.
It is crucial for the NHS to embrace better ways of working both within and across organisations. By leveraging asynchronous healthcare, healthcare organisations can enhance clinician engagement and collaboration, streamline workflows, and improve productivity, ultimately contributing to more efficient and effective healthcare delivery.
This is the first in a series of articles focusing on asynchronous healthcare, which will also look at the use of asynchronous tools to facilitate healthcare in harder to reach areas and outside of the NHS, and how to work with the NHS to make the most of asynchronous communication tools and ensure their effective use for clinicians.
