Seventy-nine percent of people would prefer not to have a first outpatient appointment and go straight to diagnostic tests if it sped up their diagnosis and treatment, a recent survey of 300 individuals[1] commissioned by Feedback Medical revealed. Their views support the new outpatient model we are delivering in partnership with Queen Victoria Hospital (QVH) through the award-nominated, straight-to-test breathlessness pathway.
Transforming the traditional outpatient model with straight-to-test pathways is a core solution identified in the government’s 2025 elective reform plan. Diverting patients away from unnecessary outpatient appointments can significantly reduce the time a patient spends on a care pathway, supporting integrated care boards to achieve the government’s target of a 5% improvement to current referral to treatment (RTT) performance.
Opinions on a revised approach to outpatients
The independent survey presented two scenarios to respondents. The first scenario outlined a traditional outpatient appointment after a GP referral, with on average 14.4 weeks to get an outpatient appointment and 6 weeks for a diagnostic test, meaning an overall wait of over 20 weeks for a diagnosis.
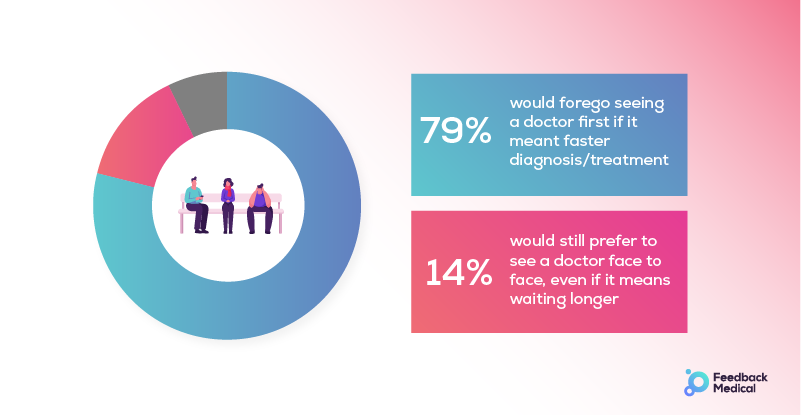
The second scenario gave the example of a straight-to-test pathway after GP referral, with the patient going for tests or scans initially and the results being reviewed by a specialist and shared with the GP. The specialist would then see the patient only if more investigations or treatment were needed. Of those surveyed, 79% would forego the initial outpatient appointment, with 14% still preferring to see a doctor even if it meant waiting longer.
“Part of our efforts to transform the approach to outpatient services is to ensure that this is in the best interests of patients. These survey results demonstrate that members of the public are supportive of not seeing a hospital consultant initially if it means that they are diagnosed and then treated more quickly – a smoother, more streamlined care pathway.
“We suspected the results might shift among older age groups to a preference for face-to-face appointments, following the public perception that older groups may not be as willing to embrace technology, but we were surprised that the opposite was true among 18-35-year-old men (33% of whom preferred to see a doctor). The figures actually increased to as much as 82% in favour of no outpatient appointment in the male aged 55+ group.”
NHS Partnerships Lead at Feedback MedicalPatient experiences of outpatient visits
Participants were asked about their experiences of visiting outpatient departments including whether they were able to choose where and when their appointment took place (64% said no), how long it took them to travel there (59% said 10-30 minutes), and how long they had to wait for their appointment (52% said 11-30 minutes).

One respondent commented: “Face to face appointments are not necessary now. If it speeds the process up then initial investigations can be done and then GP or Teams’ appointments with the consultant are preferable than taking time off work and travelling an hour to the hospital.”
In 2023 patients did not attend (DNA) nearly 7.5 million of the around 100 million booked outpatient appointments. Feedback from patients to Healthwatch in 2024 on improving outpatient services cited challenges such as a lack of choice over when and where their appointment takes place, poor administration to enable patients to reschedule and difficulty in getting to their appointment.
Reducing unnecessary outpatient appointments
The straight-to-test pathway supported by Feedback Medical at QVH in Sussex enhances diagnostic efficiency and patient care by reducing waiting times and unnecessary hospital visits. Utilising Bleepa®’s technology for asynchronous multi-disciplinary team collaboration, the project has achieved an impressive ‘diversion’ rate of 90% of referrals managed without the need for first or follow up in-person outpatient appointments.
In addition, the pathway has enabled a 63% reduction in patient waiting times from referral to treatment compared to the 18-week national target, significantly decreasing the number of patients waiting over six weeks.
This innovative approach not only improved patient experience but resulted in multiple efficiency improvements with the potential to be scaled for other pathways.
“We are working together with QVH to expand on our success across new pathways and onboarding more sites to use Bleepa® in both primary and secondary care. We are very confident that we can replicate significant impact across other areas of the NHS and support organisations to deliver against the national RTT targets set by government.”
NHS Partnerships Lead at Feedback MedicalFor more information about our work with QVH you can read our case study here or contact us here
[1] Independent survey of 300 respondents commissioned by Feedback Medical in December 2024.
